Ortoklinik & Çankaya Orthopedics, Ankara, Turkey
Total knee replacement involves resurfacing all the worn joint surfaces with metal and polyethylene implants. Bone cuts are performed to shape the surfaces and correct the deformity, and the implants of appropriate size are fixed to the cut surfaces with bone cement. Robotic total knee arthroplasty increases the accuracy of this procedure and ensures a perfect alignment and soft tissue balance. Several checks and verifications during the procedure prevents errors and documents that the desired outcome is achieved in every surgery.
What are the differences between manual and robotic total knee replacement ?
Most of the robotic systems available can only be used with a specific brand of implant, meaning that robotics cannot be used with implants from different manufacturers. Robotic systems ensure that the best fit implants are placed with a high degree of accuracy and precision, while maintaining an physiological soft tissue balance. Classical teaching in knee replacement requires to achieve a straight limb axis, with the joint line parallel to the ground. However, only 15% of the population has a straight limb, with most of the patients having a few degrees of deviation from this axis. Systematically bringing every limb, regardless of limb morphology is now believed to be one of the reasons for the small percentage of unhappy patients after total knee replacement. Personalized alignment techniques, that consider the limb morphology before the arthritis have become increasingly popular in recent years and have been shown to improve the outcomes of total knee replacement. Robotic systems with an error range of less than 1 mm and 1 degree, allow a safe and accurate execution of personalized alignment techniques, which may not always be safe with manual instruments. Restoring the pre-disease limb morphology within safe boundaries has been shown to provide a more “normal feeling” knee joint and better function after knee replacement.
Similarly, classical alignment techniques require ligament releases in 60-70% of the patients during surgery to balance the soft tissues. Extensive soft tissue releases have been shown to lead to inferior outcomes, with unnatural feeling knees and unhappy patients after knee replacement. In contrast, robotic surgery rarely requires ligament releases, and a personalized soft tissue balance can be achieved with millimetric changes in the position of the prosthetic parts that is not possible with manual instruments. Ligament releases are needed in only 3-4 % of the knees with extreme deformities in robotic knee replacement. This leads to less pain and better patient comfort after surgery, easier achievement of rehabilitation goals and a higher rate of normal feeling knee (the so called “forgotten joint”) in the long run.
Manual knee replacement requires drilling a 13-15 mm diameter, 20 cm length hole into the bone marrow canal to perform the surgery. This leads to increased blood loss after surgery and a higher risk of fat embolism from the bone marrow. In contrast, no drilling to the medullary canal of the bone is needed during robotic surgery, leading to less blood loss and lower risk of fat embolism. Unlike manual surgery, implant removal is not needed for patients undergoing robotic surgery with previous implants in the femoral canal (such as intra-medullary nails placed for fracture treatment or deformity correction). Less blood loss during and after surgery obviates the need for blood transfusions after robotic knee replacement, while less bleeding into the soft tissues leads to better knee motion and muscle strength after surgery.
Before robotic surgery
The pre-operative work-up of robotic total knee replacement is not the same as conventional surgery. A 3-D computed tomography of the involved limb is obtained and a real time model of your knee is reconstructed with a specialized software. The surgeon plans your surgery on this model in a computer, deciding on the appropriate size, alignment and placement of your implants (Figure 1). This is a preliminary plan and will be modified during surgery to balance the soft tissues. During this time, pre-anesthetic work-up including blood and urine tests, EKG and chest X-rays are performed. You should inform your physician on all your medications and allergies at this time. You will need to modify all blood thinning medication such as Aspirin and Plavix one week before surgery, your surgeon will advise on how to manage your anti-coagulation medication until the day of your surgery. You will be given instructions on antiseptic treatment of your leg one day before surgery. You will be admitted to the hospital on the day of your surgery. Regional (Epidural or spinal) anesthesia is preferred however, you can discuss other options such as general anesthesia with your anesthetist.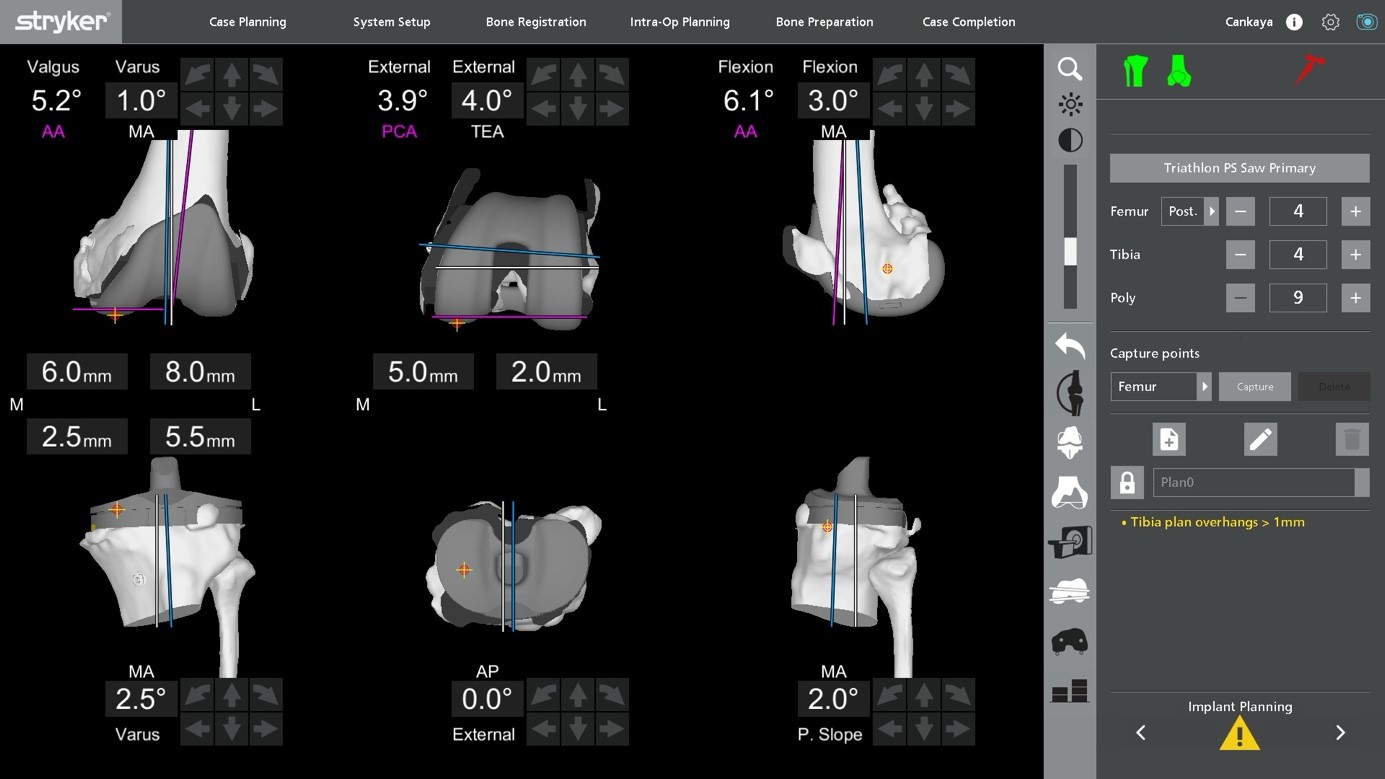
Figure 1: Pre-operative planning involves the accurate determination of size, orientation and the alignment of your total knee replacement.
Robotic total knee replacement
Robotic total knee replacement is performed in specially designed ultra-clean orthopedic operating theaters. The surgical team wears space-suits with closed ventilation systems to avoid contamination to the surgical site. Sterile, non-permeable drapes are used to cover the area and the surgical exposure is made. Optical trackers called “arrays” are placed on the femur and tibial bones using 2 pins. These arrays are the “eyes” of the robotic system and will communicate with the robot during surgery to ensure a flawless and accurate surgery.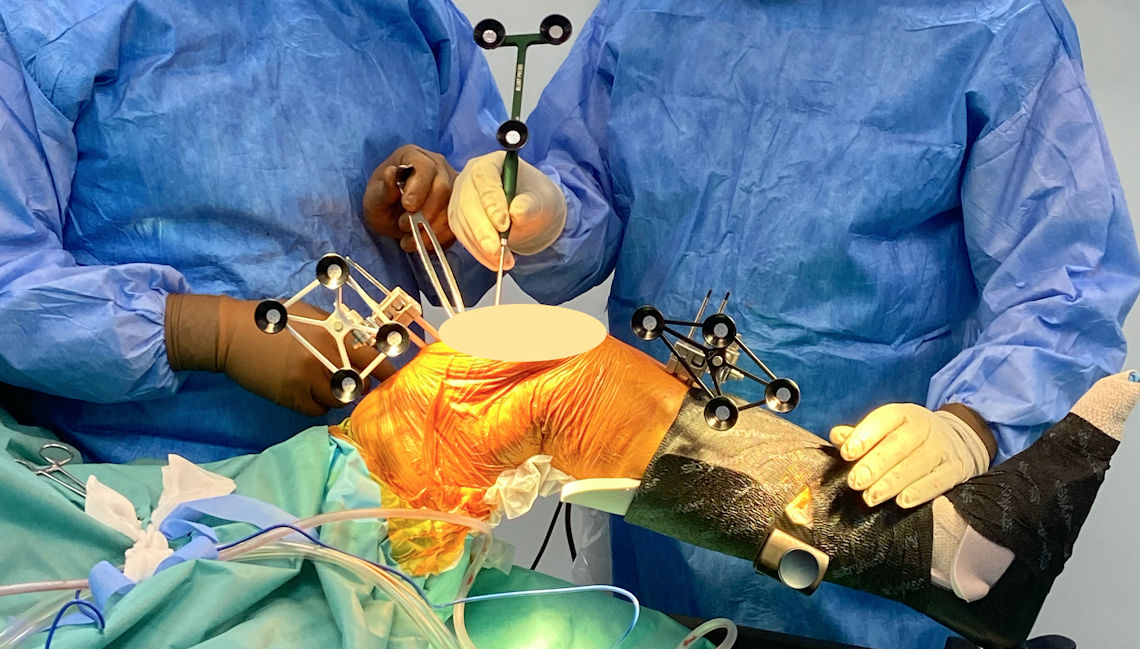
Figure 2: Placement of optical arrays during robotic total knee replacement.
The knee is defined to the robotic system by registering 64 points in the femur and tibia. This registration is transferred to the pre-operative model based on the 3D-CT scan. Once this registration process is completed, the robot knows exactly where your knee is located in space (Figure 3). The center of your hip and ankle are also registered to calculate the alignment of the whole leg.

Figure 3: Registration of bone surfaces to the robot.
Once the registration is complete, soft tissue tension is assessed with the robotic system and minor adjustments are made in the bone cuts to achieve a balanced knee. The final plan is loaded into the robotic system are bone cuts are made with the help of the robotic arm. The robotic arm is accurate to 1mm and 1 degree, and does not work outside the preset limits. The surgeon monitors the progress of the cuts on the screen and the system provides visual and audible feedback to the surgeon to ensure perfect bone cuts (Figure 4).

Figure 4: The surgeon monitors the bone cuts on screen while using the robotic arm. Figure 4: The surgeon monitors the bone cuts on screen while using the robotic arm.
Once the bone preparation is complete, trial implants are placed, verifying the size of the implants, knee range of motion and soft tissue balance. Adjustments are still possible at this stage to improve the above-mentioned points. When the surgeon is satisfied with the trial, the definitive implants are cemented to the bone surfaces. Jet lavage systems are used to obtain a clean and dry porous bone surface to provide optimal cement penetration. Antibiotic loaded bone cement is a putty like material that polymerizes and hardens in about 14 minutes. This cement is used to fix the implants to bone and provides extremely strong fixation once it hardens and allows immediate full weightbearing after surgery. A long acting anesthetic mixture is injected around the soft tissues to decrease postoperative pain and is effective up to 8 hours. Finally, the robotic arrays and checkpoints are removed, the soft tissues are sutured in layers and tranexamic acid is injected into the joint to decrease bleeding. Drains are optional and may not be needed.
After your surgery
Once you have recovered from anesthesia and regained muscle control, you can bear weight on the operated leg on the day of your surgery and stand up with help of a walker. There are no restrictions of knee movement or change of position in the bed. Pain control is achieved by intravenous or epidural patient controlled anesthesia (PCA) pumps. These devices let you control the amount of pain killers as needed and have built in safety measures prevent overdosing your medication. The PCA pumps are usually discontinued after the first day.Antibiotics are given for 24 hours to prevent implant infections, no benefit of longer antibiotic treatment has been shown. Anti-coagulants (blood thinning medication) are used for 10-30 days depending on your risk profile to prevent blood clots forming in your legs. These can be in the form of tablets such as Aspirin or Xarelto or self-administered injections under the skin.
Physical therapy under the supervision of a physiotherapist is begun on the day of your surgery. Your surgeon may prescribe the use of a continuous passive motion (CPM) device, which moves your knee in a controlled manner. These devices may also be used at home if your surgeon deems necessary. Stair climbing exercises begin on the second day and you will be free to walk around with a walker or a similar assistive device. An X-ray of your knee is taken on the second day (Figure 5). Drains are removed at 24 hours if used.

Figure 5: X-ray images of the knee of a patient with advanced arthritis before and after robotic total knee replacement.
You will be given an “implant passport” containing information and the barcodes of all the implants placed in your knee. It is essential that you keep this passport in a safe location since it contains essential information regarding the type and properties of your implants should the need for a change of parts rise in later years. You can also document that you have metal implants in your body for airport security and metal detectors.

 TÜRKÇE
TÜRKÇE



